People with disabilities can live a full life, but the key is achieving and maintaining health and wellness. The U.S. Surgeon General’s “call to action” report, published in 2005, illustrates this vital connection, yet presents significant health disparities for people with disabilities including access to care, risk factors, and outcomes.

In the Accessible Designs for Personal Health Records project, three organizations are working together to demonstrate that designing specifically for people with disabilities can lead to electronic Personal Health Records (PHR) that are not only accessible, but are innovative, useful, and beneficial for everyone.
The project goal is to demonstrate a user-centered design process in creating prototypes for an accessible PHR. The team engaged almost 200 people with disabilities in requirements gathering, iterative design, and user testing. The project will be completed in late 2014 and all materials, including methods, results, specifications, code, and designs, will be shared for public use.
Building on a Foundation of Goals
Living a full life is achieved by setting and meeting personal goals. Understanding a person’s goals is also important to healthcare providers. Goals connect each person to their health and wellness needs, as well as their social and emotional needs, all of which are vital to decision-making between patients and providers.
The first discussion with participants focused on goals. Responses echoed the Surgeon General’s report with every participant having the goal to live independently in every area of life including education, work, home, mobility, and relationships with family and friends.
When asked about the connection between goals and health, participants said health was the most important factor in achieving and maintaining independence. Many participants shared experiences where health setbacks threatened all the work they had done to achieve independence. When discussing how they could manage health toward meeting their goals, participants described an extensive list of experiences with highly detailed and sophisticated ideas on how information, communication, and technology could be applied to a wide range of health scenarios.
It wasn’t surprising that participants’ vision of an ideal PHR was far beyond what is currently available. Many participants manage multiple complex health issues, both related and unrelated to their disability, compounded by challenges in mobility, communication, income, and access. It is important to realize that a disability is not an illness. Many participants felt they were in good health and did not consider their disability a health issue. However, nearly all participants expressed dissatisfaction with healthcare system access and health information resources.
The remainder of this article illustrates examples of potentially innovative PHR designs discovered with project participants.
Patient Education for Everyone
There is no shortage of online medical education content, but finding accessible content is a challenge. Instead of searching the web, participants demanded trusted sources of educational medical content integrated with their medical record. While none of the participants were clinical informatics researchers, their ideas reflected current topics, such as “information prescriptions” written by providers and context based “info buttons” providing on-demand definitions for diagnoses, labs, medications, or any medical terminology in their record.
Accessible content is particularly important for people who are blind or visually impaired, but other participants were equally passionate about bringing attention to their concerns. For example, some people who are deaf may prefer video presentations in American Sign Language (ASL) versus captioned videos

Fortunately, patient education is a major focus of U.S. government healthcare incentive programs, and many commercial patient portals can be integrated with multiple education resources. To provide accessible content, the team built on an approach developed by our project leading organization—public broadcaster WGBH—that combines accessibility with information architecture techniques designed to improve search and retrieval.
WGBH developed an accessible K-12 education portal built on tagging the metadata of content by subject as well as media type. When users search for content, media tags support filtering based on accessibility preferences. Using this system, a person who is deaf can set a preference for videos with captions, while a person who is visually impaired can set preferences for images or charts with descriptive text. By following the same approach, a PHR could deliver appropriate information in the best format for the person searching for health information. However, it is highly unlikely that any single source of medical education content will be fully accessible to all people with disabilities. Ideally, PHRs could be connected to multiple resources with some specializing in a particular form of content. For example, DeafMD.org (see Figure 2) is a unique and innovative resource of medical education content that provides ASL videos on a growing collection of health topics.
The Pew Research Internet Project reports that 72 percent of Internet users searched for health information within the previous year. Given this, we feel this approach could benefit all users. For example, media tags could be used to filter medical education content by learning style preference (text, visual, auditory, and/or video), content for children, reading level, level of detail, and language.
An Interactive, Patient-Centered Care Plan
Many people with severe physical disabilities rely on a care plan: detailed instructions and goals for daily health and wellness activities developed collaboratively with a person’s care team. However, most are written in a highly clinical format and lack practical information required by patients, their caregivers, and family members (See Figure 3).

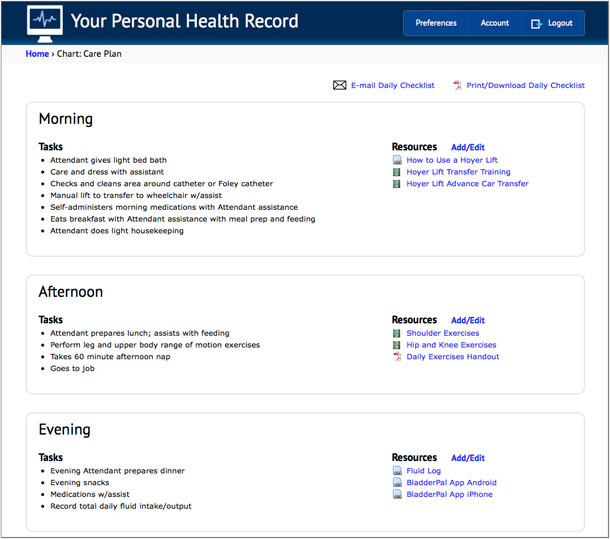
The prototype PHR includes a patient-centered care plan that enables the patient, or anyone involved in his or her care, to attach personalized content that provides additional information for each task (see Figure 4). This could be an existing resource or content created directly by the patient or their care team. For example, a YouTube video demonstrating the proper use of a patient lift, a smartphone video of a physical therapist performing an exercise, or a link to an app to track daily fluid intake and output.
Care plans are not just for people with disabilities. They are important for people recovering from surgery, or those managing asthma, diabetes, or any chronic illness. One participant, a woman who is paraplegic, said this care plan would be useful for her own care, but even more so by helping her manage the care of her aging, diabetic mother.
To demonstrate that this care plan works for anyone, we used the same design strategy to create a plan for a child with asthma that included instructions, an animated presentation for children, videos demonstrating the proper use of an inhaler, and content on managing environmental triggers. Another participant, a woman with a cognitive disability, did not have a care plan, but told us this design would be extremely useful in helping her manage her daughter‘s asthma.
Medical Equipment as Part of the Medical Record
Many of the participants with severe physical disabilities depend on an array of medical equipment such as adjustable beds, shower chairs, special pads to prevent bedsores, patient lifts, and more. For many, their most important equipment is the power wheelchair. The power wheelchair is critical to mobility and, therefore, independence. These chairs are marvels of technology and engineering, and many are highly customized to the user. Some even provide wireless integration with computers, smartphones, and home automation. Like any expensive technology (some can cost more than $30,000), service and repairs are inevitable.

Unfortunately, participants described many difficulties in servicing their chairs (and other equipment) that lead to highly stressful situations that often jeopardize their independence. For example, if their chair does not function, a person can’t go to work, resulting in trouble paying their monthly bills and maintaining their residence. In the U.S., equipment maintenance is further complicated by cumbersome insurance approval processes and paperwork.
For example, one participant’s chair had two issues: it needed new tires and the joystick controller was malfunctioning. Each issue needed to be addressed by separate service vendors. To receive insurance approval and payment, the first thing the user needed was a prescription from his physician. Without an electronic record or mobility, he had to wait a few days to receive the prescription by mail. After receiving the prescription, he was then able to contact the vendors, but he also needed to provide each vendor with extensive information on his chair including multiple model numbers, serial numbers, repair history, and details on all customizations.
The team found only two existing PHR systems that addressed equipment, but both provided inaccessible functionality limited to surgical implants (for example, pacemakers and artificial hips.) To support a broader range of equipment scenarios, the PHR prototype provided a database where the patient, or anyone involved in his or her care, could enter and track all equipment information, add attachments, and share this information with their providers. During testing, participants offered more ideas on extending the system to manage medical supplies such as urinary catheters, syringes, and more. Some participants went even further, suggesting integrating the supply list with cost comparisons and online ordering.
People with severe physical disabilities aren’t unique in relying on medical equipment or supplies, but addressing their complex requirements led to versatile designs that could benefit others, including a person in a home care situation, the parent of a child with a chronic illness, or a person with diabetes who uses a glucose meter and administers their own insulin shots.
Summary
These three examples of a PHR designed for people with disabilities demonstrate that addressing their needs results in systems that are useful for everyone. However, these examples represent only three of more than twenty use cases for PHR functionality that were identified in the project. Like the examples presented here, each provides detailed functionality well beyond the capabilities of existing systems.
People with disabilities face barriers in health, wellness, and technology. Meanwhile, healthcare is undergoing a massive transformation with the goal of developing technology to support and improve every area of care. Designing for those who are among the most underserved by technology and the healthcare system demonstrates a strategy that can contribute to achieving the ambitious goal of improving all areas of healthcare for everyone.
[bluebox]
Project Partners
“Accessible Designs for Personal Health Records” is a federally funded research and development project (grant #H133G110095, U.S. Department of Education, National Institute on Disability and Rehabilitation Research). The project is a collaboration of WGBH’s National Center for Accessible Media, the Inglis Foundation, and The Children’s Hospital of Philadelphia, Center for Biomedical Informatics.
Boston public broadcaster WGBH’s Carl and Ruth Shapiro Family National Center for Accessible Media (NCAM) is the project leader and grant recipient. NCAM is a non-profit R&D organization dedicated to achieving media access equality for people with disabilities. NCAM provides accessibility consulting to major media corporations and government policy makers. WGBH team: Larry Goldberg, principal investigator; Donna A. Danielewski, Ph.D., director NCAM; Madeleine Rothberg, project director; Geoff Freed, accessibility expert; and independent contractor Jason Withrow, prototype developer.
Inglis Foundation is a Philadelphia-based organization that been managing the care of people with disabilities for 150 years. Inglis maintains a 300 bed long term care facility specializing in the care of people with severe physical disabilities. They also manage the care of nearly 1,000 people with disabilities living in the community. Inglis team: Gavin Kerr, CEO; Lea Frontino, VP of innovation, and Dawn Waller, director adapted technology program.
The Children’s Hospital of Philadelphia (CHOP) is the first U.S. hospital dedicated to the care of children and is home to one of the largest pediatric research programs in the country. The Center for Biomedical Informatics (CBMi) develops and studies health information technology for clinicians, patients, and families. CHOP-CBMi team: Robert Grundmeier MD, director of clinical informatics and Dean Karavite MSI, lead human computer interaction specialist. [/bluebox]
[greybox]
Text from Figure 3: Extract from a 5 Page Care Plan
Goal (Desired Outcome), Identified Need, Action Step/Service, Provider/Responsible Party, Preferences
Transfers, Assistance with transfers, PCA to transfer consumer from/to bed, shower chair, wheelchair and sofa daily, PAS, Consumer has chosen model of service
Frequency/Duration (Hours/Days): 1 hr/day, 7 days/week. Mon 1.00, Tues, 1.00, Wed 1.00, Thurs 1.00, Fri 1.00 Sat 1.00, Sun 1.00
Total Hours/Week: 7, Any Barriers/Risks: Consumer is at risk of falls while…, Mitigation Strategy: Consumer states he utilizes lift and will…, Agree/Disagree: Agrees
Goal (Desired Outcome), Identified Need, Action Step/Service, Provider/Responsible Party, Preferences
Maintain flexibility, Assistance with ROM, PCA to assist with arm and leg stretches 2x/day for 30 minutes, PAS, Consumer has chosen model of service
Frequency/Duration (Hours/Days): 1 hr/day, 7 days/week. Mon 1.00, Tues, 1.00, Wed 1.00, Thurs 1.00, Fri 1.00 Sat 1.00, Sun 1.00
Total Hours/Week: 7, Any Barriers/Risks: Consumer is at risk of injury if ROM is…, Mitigation Strategy: Consumer states he train attendants…, Agree/Disagree: Agrees
[/greybox]
[greybox]
Text from Figure 4: Your Personal Health Record
Morning Tasks
- Attendant gives light bed bath
- Care and dress with assistance
- Checks and cleans area around catheter or Foley catheter
- Manual lift to transfer to wheelchair w/assist
- Self-administers morning medications with Attendant assistance
- Eats breakfast with Attendant assistance with meal prep and feeding
- Attendant does light housekeeping
Resources Add/Edit
- How to Use a Hoyer Lift
- Hoyer Lift Transfer Training
- Hoyer Lift Advance Car Transfer
Afternoon Tasks
- Attendant prepares lunch; assists with feeding
- Perform leg and upper body range of motion exercises
- Takes 60 minute afternoon nap
- Goes to job if works (1-5pm)
Resources Add/Edit
- Shoulder exercises
- Hip and knee exercises
- Daily exercises handout
Evening Tasks
- Evening Attendant prepares dinner
- Evening snacks
- Medications w/assist
- Record total daily fluid intake/output
Resources Add/Edit
- Fluid Log
- BladderPal App Android
- BladderPal App iPhone
[/greybox]残障人士面临技术和健康保健方面的困难。尽管网上存在丰富的医学教育内容,但是查找具有可访问性的内容往往很难。在健康保健内容从印刷版向网络版的过渡中,满足残障人士的需求是必不可少的步骤,面向残障人士的设计应该具有额外的优势。要将可实现患者目标的信息、沟通和技术完美地组合起来,以允许个人成功地管理和维护自己的健康与独立能力。 文章全文为英文版
장애인들은 과학기술과 의료에 있어 난관에 처합니다. 의료 교육 콘텐츠가 온라인 상에 수없이 많기는 하지만, 접근 가능한 콘텐츠를 찾기가 쉽지 않습니다. 의료서비스가 인쇄물에서 온라인으로 변화되고 있기 때문에 장애인들의 요구에 부응하는 것이 아주 중요합니다. 또한 장애인을 위한 설계는 추가적인 이점도 있습니다. 환자들의 목표를 해결하기 위해 정보와 의사소통과 기술을 훌륭히 결합하면 사람들이 자신의 건강과 독립성을 성공적으로 관리하고 유지할 수 있도록 도움을 줍니다. 전체 기사는 영어로만 제공됩니다.
Indivíduos com deficiências enfrentam barreiras na tecnologia e nos serviços de saúde. Embora exista um vasto conteúdo educacional médico on-line, encontrar conteúdo acessível geralmente constitui um desafio. À medida que o sistema de saúde migra do material impresso para o material on-line, atender às necessidades de indivíduos com deficiências torna-se fundamental e projetar para indivíduos com deficiências apresenta uma vantagem adicional. Uma combinação bem-sucedida de informações, comunicação e tecnologia para atender aos objetivos dos pacientes permite que os indivíduos administrem e mantenham sua saúde e independência satisfatoriamente. O artigo completo está disponível somente em inglês.
障害がある人は、テクノロジーと医療の両面において障壁に直面するものである。医療教育に関する様々なコンテンツがオンライン上に存在する一方で、アクセス可能なコンテンツを探すことは困難な場合もある。医療が印刷物からオンラインへと推移する中、障害者のニーズを満たすことは不可欠なことであり、また障害者のためにデザインすることには付加価値がある。情報、コミュニケーション、テクノロジーをうまく組み合わせて患者の目標達成を支援すれば、各自が自らの健康を管理して自立した生活を送ることができるのである。 原文は英語だけになります
Las personas con discapacidades se enfrentan a barreras en la tecnología y la atención médica. Si bien existe una gran cantidad de contenidos de educación médica en línea, encontrar contenido accesible suele ser un desafío. A medida que la atención médica realiza la transición de documentos impresos a en línea, es esencial cumplir con las necesidades de las personas con discapacidades y diseñar para estas personas tiene una ventaja adicional. Una combinación exitosa de información, comunicación y tecnología para abordar las metas de los pacientes permite a los individuos gestionar y mantener con éxito su salud e independencia. La versión completa de este artículo está sólo disponible en inglés
