With several notable exceptions, much of the early research on the use of technology was justified on the basis of increased access, such as electronic contact for a natural extension of face-to-face dialogue, and the computerization of self-help materials. Increased engagement and improvements in the effectiveness of treatment have received less attention. Collaboration between human-computer interaction (HCI) and mental health professionals can help to maximize the effectiveness of new technologies. While mental health professionals have the necessary domain expertise, HCI professionals are experienced in design methods and are likely to have a broader knowledge of the potential uses of new technologies. For example, the experience of HCI researchers is important given the high cost of systems failures in sensitive interventions. Other ongoing areas of HCI research, such as designing for personal reflection and behavior change, can play a valuable role in future research on mental health technologies.
Examples of Exploratory Systems
In our own research we have primarily focused on the design of interactive systems to support talk-based, or psychological, approaches to mental health treatment. Over the past five years we have developed several exploratory systems:
Personal Investigator
Personal Investigator (PI) (see Figure 1) is a 3D computer game designed to support adolescent mental health interventions. It incorporates Solution Focused Therapy, a goal-oriented, strengths-based intervention approach. PI is used in clinical sessions involving one therapist and one adolescent. It aims to ease the difficulties many adolescents experience in engaging with face-to-face treatments. Two clinical evaluations of PI have been conducted, the first with four adolescents, the second with twenty-two. Results indicate that PI can have a beneficial impact on interventions, supporting improved client-therapist relationships and improved client engagement.

PlayWrite
PlayWrite extended the ideas developed with PI. Rather than providing a fixed game, it provides a flexible game template and enables end users—mental healthcare (MHC) professionals—to create and adapt the content delivered through this template. Using PlayWrite, MHC professionals have created ten games, implementing different theoretical approaches to MHC and targeting a range of difficulties including depression, anxiety, and anger management. For example, gNat’s Island supports a six-week cognitive behavioral therapy (CBT) intervention for depression.
Mobile Mood Diary
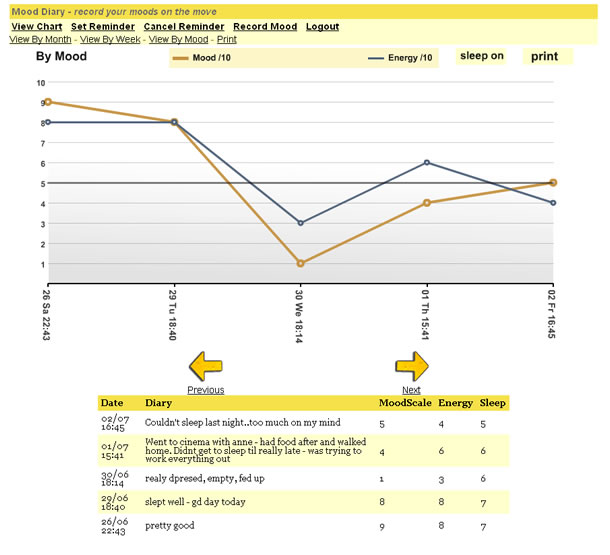
Therapists, particularly those practicing CBT, often ask clients to complete paper-based mood charts, but adherence can be low and they can provide unreliable information. Mobile Mood Diary, a mobile phone- and computer-based mood chart system (see Figure 2), was developed to make recording moods more convenient and reliable. A controlled school study was run studying compliance variation between a paper-based chart and the Mobile Mood Diary. An initial clinical evaluation with ten adolescent clients has also been completed. Results showed a high level of adherence amongst participating adolescents over a sustained period.
Design Challenges and Future Directions
A more detailed description of previous work in mental health technologies is available in Computers in Talk-Based Mental Health Interventions by Coyle et al, and Hands-on Help: Computer-aided Psychotherapy from I. M. Marks. We conclude this article by considering several significant challenges for future work in this area.
Theories for Design and Evaluation
Mental health technologies remain a relatively unexplored design space. Alongside exploring the potential of a wider range of technologies, there is a need for more detailed investigation of theories, from both the mental health and HCI domains, which can help to generate ideas and support us in reasoning about designs. For example, mental health frameworks such as the Skilled Helper Model provide a structured overview of a helping intervention. Behavior change models such as the Trans-Theoretical Model may also prove useful, as could activity theory, which has previously been applied to a range of healthcare settings. Applying models for complex medical evaluations may also prove beneficial.
Strategies for Collaborative Design
While collaboration with domain experts and end users is important in many design areas, it has a particular significance in mental health areas. The ethical requirements and stigma associated with mental health means that designers often face severe restrictions on access to people experiencing difficulties and to situations in which interactive systems will be used. Faced with such constraints, HCI practitioners may have to rely on the expertise and insights of mental health professionals. However, research in related healthcare areas has shown that the success of interdisciplinary teams is not something that can be taken for granted. We have discussed initial strategies for collaborative design decision making in our paper “Clinical Evaluations and Collaborative Design: Developing New Technologies for Mental Healthcare Interventions.” We need to build a deeper understanding of collaborative design strategies, and develop techniques which support effective interdisciplinary teams.
Adaptable Systems
Therapists often work with clients from different socio-cultural backgrounds, experiencing a range of disorders of varying severities. Furthermore, teams of therapists often have different theoretical backgrounds and adopt a variety of eclectic approaches to working with clients. In such situations, fixed systems offer limited benefits. Systems where the core capabilities are reusable across a range of situations, and which can be adapted to the needs of end users, would be more useful. PlayWrite represents an example of such a system. In this case, mental health professionals play an active role in adapting the system. This approach can also help to support collaboration.
Support for Resource Allocation Strategies
Better targeting of resources and needs-based service provisions have become important goals in mental health service delivery. Models such as Stepped Care encapsulate this notion, with distinct steps—intensities of treatment—ranging from inpatient treatment, through primary care teams, dealing with issues such as mild depression to general practitioners supporting initial contact and diagnosis. Designing interactive systems to support these different levels of care, and transitions between them, represents a major challenge.
